WE SOLVE YOUR DOUBTS AND CONCERNS ABOUT GLAUCOMA
952 47 83 42
What is glaucoma?
We call glaucoma to a set of conditions, in which there is an injury of the optic nerve, as a consequence of an elevation of the ocular pressure.
Glaucoma damages optic nerve fibres usually slowly and progressively, and if treatment is not established it can lead to blindness.
Why is it necessary for the eye to have a tension?
In order to see, the eye is transparent in its visual axis, so that light can pass through it and reach the retina. This is achieved, among other structures, thanks to the existence of the aqueous humour.
The aqueous humour is generated in the ciliary processes, and drains through another structure that is like a drain, called the trabecular meshwork. In this way there is a balance between formation and drainage that maintains the eye at an optimum tension, if this were too low the eye would lose its shape and would see very badly, and if it were higher glaucoma would appear.
.
In glaucoma, what happens is that the pressure acts on the entire eye, damaging its most sensitive part, which is the head of the optic nerve or papilla.
Symptoms of glaucoma
Glaucoma does not usually affect vision in the early stages of the disease, at least in a way that the patient is aware of. When it is very advanced, it constricts the visual field, limiting the ability to move, and eventually leads to blindness.
If the pressure is too high, it can be painful, cause nausea and vomiting and coloured halos.
Types of glaucoma
Primary open-angle glaucoma
It is by far the most common glaucoma. Its prevalence increases with age, and it has a significant genetic basis. This is important because patients' immediate family members should be screened for the disease. It rarely appears before the age of 40. The progression is usually slow, and the optic nerve gradually loses fibres until vision is lost. In its diagnosis, it is important to carry out visual fields, which is where the optic nerve lesion is best expressed, as well as imaging tests to directly study the papilla, such as papillary oct.
Congenital and infantile glaucomas
These are special types of glaucoma that appear at birth in the case of congenital glaucoma and in children in the case of infantile glaucoma. Their prognosis is worse because they appear at a very early age.
Normal tension glaucoma
It is a variant of the previous one, where the pressure is at normal levels.
Primary angular closure glaucoma
There is a closure of the outflow of aqueous humour through the peripheral iris, which raises ocular pressure. It can occur acutely or chronically. It can be prevented by laser iridotomy.
Secondary glaucomas
There are several secondary glaucomas that can occur, but they are much less frequent. Generally speaking, their treatment will be that of the cause of the glaucoma.
Diagnosis of Glaucoma
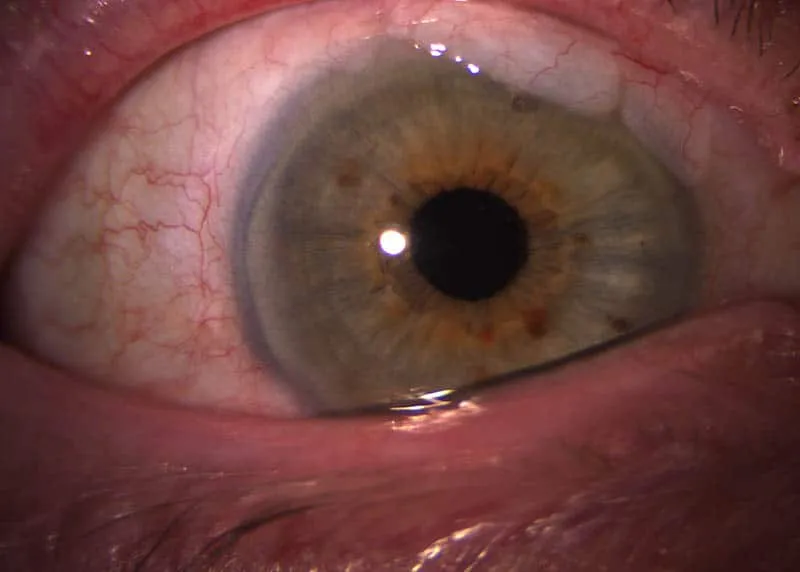
For the diagnosis of glaucoma, a detailed history is important, including the presence or absence of family history, as well as an examination, which includes taking intraocular pressure, a study of the anterior pole of the eye to rule out secondary causes and to determine whether the glaucoma is open or closed angle, gonioscopy and examination of the papilla or head of the optic nerve.
In glaucoma, the following are essential diagnostic tests.
Tonometry
Tonometry is the taking of eye pressure. Although normal pressure is considered to be up to 21 mm Hg, this is relative, as there are eyes with higher pressures that do not develop glaucomatous damage, and conversely eyes with lower pressures that do develop glaucomatous damage. It is very important, but by itself it is not enough to establish the diagnosis, unless the pressure is very high, above 29 mm Hg, a pressure at which, even if there is no damage to the optic nerve, there is consensus on the need for treatment.
It is an easy, risk-free test that is routinely performed in ophthalmology practices.
Campimetry
This is the main test performed in glaucoma, together with tonometry, and is useful not only for diagnosis but also for monitoring the possible progression of glaucomatous damage.
Gonioscopy
Gonioscopy is the observation of the anterior chamber angle. It is used to assess whether a glaucoma is open or closed angle. It is also essential for applying laser to the trabecular meshwork.
Optical coherence tomography of the optic nerve.
Together with other imaging tests (GDX, HRT), it is used to measure the number of optic nerve fibres, and together with campimetry it helps us to assess the progression of glaucoma.
Corneal pachymetry
Corneal pachymetry involves measuring the thickness of the cornea. It is useful in the management of glaucoma because particularly thin corneas give falsely low pressures and very thick corneas give falsely high figures. This is important because a person with a very thick cornea may lead us to believe that their pressure is pathological when in fact it is normal, and more importantly may lead us to believe that a pressure in a very thin cornea is normal, and that we do not diagnose glaucoma, at least at an early stage. The latter situation occurs in myopic patients who have undergone Excimer laser surgery, as the cornea is surgically thinned.

Glaucoma treatment
The main strategy in the treatment of glaucoma will be to control intraocular pressure so that glaucomatous damage does not progress, or at least slows down and does not lead to blindness.
Several therapeutic resources are available for this purpose:
Medical treatment.
There are various pharmacological groups, which can be combined with each other. However, we must not forget that they have their side effects, and that as few drugs as possible should be used.
The groups include prostaglandin derivatives, beta-blockers, alpha-2 agonists, topical carbonic anhydrase inhibitors and miotics. All of them are applied in the form of eye drops. They are usually applied for years and in most cases it is possible to control glaucoma with these drugs.
We also have oral treatment with carbonic anhydrase inhibitors, which are usually used for short periods of time, to control transient ocular hypertension or while awaiting surgery.
Laser treatment of glaucoma
Laser trabeculoplasty
Can achieve pressure drop of 10-40%. It tends to lose efficacy over time. Equivalent to putting a drug in eye drops.
Laser iridotomy.
It is performed in narrow-angle glaucoma, either to prevent or to treat angular closure.
Diode laser cycloablation.
It is usually done in the operating theatre, under regional anaesthesia.
Laser iridoplasty.
It is performed on eyes with a narrow chamber to deepen the angle.
Trabeculectomy.
With this technique we manage to lower the pressure by creating a protected fistula. It is indicated when it is not possible to control the progress of the disease with eye drops or when the disease is diagnosed in an advanced stage and we need to lower the pressure considerably. In this case, early surgery may have a better long-term prognosis than pharmacological treatment.
Non-penetrating glaucoma surgery (non-perforating sclerectomy)
It has fewer operative complications than trabeculectomy, but usually achieves less pressure relief than trabeculectomy.
Drainage devices
Because they are valves, they are generally reserved for glaucomas with a poorer prognosis.
Laser iridoplasty.
It is performed on eyes with a narrow chamber to deepen the angle.
Mini-shunt express implant
In our ophthalmology clinic in Fuengirola we have experience and good results with the mini-shunt express implant, which achieves intraocular pressure control similar to trabeculectomy, although with fewer operative complications. The surgery is performed in Benalmadena at Hospital Vithas and in Malaga at Hospital El Angel.
Surgical treatment of glaucoma
Glaucoma Prevention
Can we prevent glaucoma?. There is really little we can do to prevent the onset of glaucoma. It is advisable to have an adequate weight, not to smoke, to control blood pressure and not to drink too much caffeine. Physical exercise lowers eye pressure, at least while you are doing it.
The most important thing would be to make an early diagnosis, and for this, as the disease does not usually show symptoms in its early stages, an appropriate ophthalmological examination is essential. Early diagnosis makes it easier for the disease to be treated earlier and gives it a better prognosis.
If we are diagnosed with glaucoma, we must inform all our immediate family members so that they can be checked to rule out the disease.
Risk Factors
The risk factors for primary glaucoma of open angle are:
- High eye pressure, the higher the higher the risk of developing glaucoma.
- Age. More common in the elderly.
- Race. It is more common and more severe in the black race.
- Family history of glaucoma
- Diabetes mellitus
- Myopia
- Large optic papillae
The only risk factor we can act on is eye pressure through treatment.
Questions about Glaucoma
Is ocular hypertension the same as glaucoma?
No. Ocular hypertension is when there is elevated pressure in the eye but no damage to the optic nerve, therefore, no glaucoma.
I have been diagnosed with glaucoma, will I go blind?
The key to treatment is to prevent the progression of optic nerve damage. If we manage to keep the pressure at low levels, there will be no progression and vision will be preserved. Early diagnosis and correct treatment are important.
If I have ocular hypertension, will I develop glaucoma?
Some patients with ocular hypertension will develop glaucoma, but not all.
I have glaucoma, do I need surgery?
Some glaucomas require surgery for control, but most of them can be controlled with medical or laser treatment, although sometimes surgery is necessary if this is not achieved.

